Gastric band surgery is not outdated, yet it is one of the legacies of the bariatric surgery whose drawbacks can be understood only in the long run, upon the patient compliance rates and the success rates of revision. Patients are more likely to make a better choice based on the durability, and lifestyle effect- not reversibility.
Unless you are doing research on gastric band surgery, most likely you are seeking a less radical, and possibly safer way to lose weight. That is what most pages promise. The issue lies in the fact that a lot of explanations end with the mechanism of the surgery and do not take into consideration what transpires a few years after. The agitation arises at the point when patients find out too late that reversibility is not reliability, and success over the long term requires follow-up, tolerance, and behavioral fit.
The fact of the matter: gastric band surgery may be effective in a limited population of patients, but in the vast majority of people in the current era, it is less permanent in weight loss and more likely to be revised than newer bariatric procedures. Realizing that the initial investment is the variant between an informed choice and an irritating one.
Key Takeaways
- Gastric band surgery is the least invasive bariatric option, but also the least durable long-term.
- High adjustment, revision, and removal rates are the main reason its use has declined.
- “Reversible” sounds reassuring, but often means additional procedures later.
- Long-term costs can exceed expectations due to follow-ups and complications.
- It may suit a small subset of patients—but it is no longer the default choice.
What Is Gastric Band Surgery?
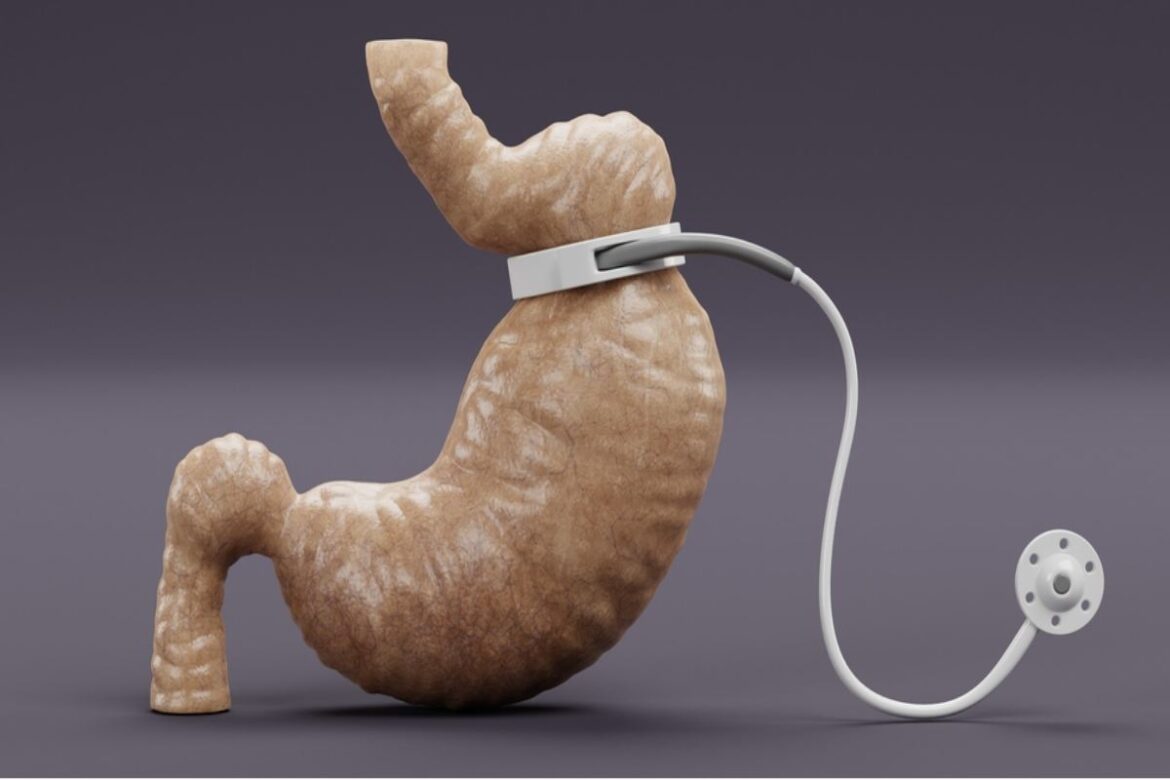
Gastric band surgery, often called lap band surgery, involves placing an adjustable silicone band around the upper part of the stomach. This creates a small pouch that fills quickly, helping you feel full after eating less.
Unlike other bariatric procedures:
- No part of the stomach is removed
- Digestion remains normal
- Weight loss relies entirely on restriction and behavior change
The band can be tightened or loosened through saline injections during follow-up visits. In theory, this adjustability allows weight loss to be customized over time.
Key distinction: gastric band surgery restricts intake but does not change hunger hormones in the way sleeve gastrectomy or gastric bypass does. That difference matters long term.
Who Is Gastric Band Surgery Actually For?
This is where many articles become vague. In practice, gastric band surgery works best only when several conditions line up.
Typical eligibility
- BMI generally above 35, or above 30 with obesity-related conditions
- Willingness to attend frequent follow-ups
- Comfort with slow, incremental weight loss
Behavioral and psychological fit
- Strong portion control discipline
- Low tolerance for snacking or liquid calories
- Ability to follow structured eating rules long term
Poor candidates (often not stated clearly)
- People seeking rapid or guaranteed weight loss
- Those with inconsistent follow-up habits
- Patients with reflux-dominant symptoms
- Anyone uncomfortable with the idea of future revision surgery
This reinforces the central POV: success depends more on patient fit than on the device itself.
Weight Loss Results Over Time
Short-term results (first 1–2 years)
The majority of patients undergo a progressive weight loss, which usually is less rapid than the one seen with sleeve or bypass surgery. The initial findings may be satisfactory, particularly when the follow-ups are regular.
Long-term reality (5–10 years)
This is where outcomes diverge. Many patients:
- Plateau earlier than expected
- Regain weight despite band adjustments
- Develop intolerance that limits band effectiveness
Illustrative scenario:
Two patients lose similar weight in year one. By year five, the sleeve patient maintains most of it, while the band patient struggles with adjustments, eating discomfort, or regain. This pattern explains why long-term satisfaction differs.
Qualitative comparison
| Procedure | Long-term weight stability | Maintenance difficulty |
| Gastric Band | Low to moderate | High |
| Gastric Sleeve | High | Moderate |
| Gastric Bypass | High | Moderate |
Risks, Complications, and Band Removal
Common complications
- Band slippage
- Band erosion into the stomach
- Chronic nausea or vomiting
- Difficulty swallowing solid food
Revision and removal
Many patients eventually require:
- Band repositioning
- Complete band removal
- Conversion to sleeve or bypass
This is why professional bodies such as the American Society for Metabolic and Bariatric Surgery (ASMBS) and NICE (UK) have noted declining usage trends.
Why “reversible” can mislead
Reversibility sounds like safety. In reality, it often means:
- More procedures over time
- Higher cumulative risk
- Greater lifetime cost
Gastric Band vs Sleeve vs Bypass
Rather than features, outcomes matter most.
| Factor | Gastric Band | Gastric Sleeve | Gastric Bypass |
| Invasiveness | Lowest | Moderate | Highest |
| Hormonal effect | None | Yes | Yes |
| Long-term durability | Low | High | High |
| Revision likelihood | High | Low | Low |
| Follow-up burden | High | Moderate | Moderate |
This comparison explains why many surgeons now recommend sleeve gastrectomy as the first-line option for most patients.
Cost of Gastric Band Surgery by Country
| Country | Typical upfront range | Long-term cost considerations |
| United States | Higher | Adjustments, imaging, revisions often add significantly |
| United Kingdom | Moderate | Limited availability, follow-up variability |
| India | Lower | Medical tourism costs, long-term access planning |
Organizations like the World Health Organization (WHO) and NHS England emphasize long-term outcomes when evaluating bariatric procedures—not just initial price.
Why Gastric Band Surgery Is Declining Worldwide
Several forces drive this shift:
- Surgeons observe higher revision rates over time
- Patients report lower satisfaction at long-term follow-up
- Newer procedures offer better durability with similar risk profiles
Many bariatric centers now reserve gastric band surgery for exceptional cases rather than standard treatment.
Is Gastric Band Surgery Still Worth It in 2026?
It may make sense if:
- You want the least invasive option possible
- You accept slower, less predictable weight loss
- You are comfortable with ongoing adjustments
It usually does not if:
- You want durable, long-term results
- You prefer fewer follow-ups
- You want hormonal appetite changes
A Simple Decision Framework for Patients
Ask yourself:
- Can I commit to years of follow-ups?
- Am I comfortable with a higher chance of revision?
- Do I value reversibility more than durability?
If most answers lean toward durability and simplicity, newer procedures are usually a better fit.
Conclusion
Gastric band surgery will not be completely eliminated- but it is not the simple-solved dish as many articles have made it to be perceived. When we compare it by its results in the long run, its burden on lifestyle, and its risk of revision, the reasons that led to its decline in popularity are evident. The least invasive option is not the best, but the one that is in line with realistic expectations and sustainable outcomes.
Trust Note
This article is informed by international bariatric guidelines, long-term outcome reviews, and consensus trends from organizations such as ASMBS, NICE, and WHO. The focus is outcome-first decision support, not promotion.