Gamma-aminobutyric acid (GABA) supplements have gained popularity for anxiety and sleep support, but their effectiveness is limited by the blood-brain barrier. Current evidence suggests potential peripheral and gut-mediated benefits rather than direct brain effects.
About the Author and Medical Review
Dr. Anika Sharma, PhD, Neuroscientist
Dr. Sharma is a neuroscientist specializing in neuropharmacology at Stanford University School of Medicine, with over 12 years of research experience studying neurotransmitter systems. She has published 34 peer-reviewed articles on GABAergic signaling in journals including Nature Neuroscience and Journal of Neuroscience. Dr. Sharma serves on the editorial board of Neuropharmacology and regularly reviews grant applications for the National Institutes of Health.
Medical Reviewer: Dr. Benjamin Chen, MD
Board-certified psychiatrist and clinical pharmacologist at Massachusetts General Hospital, specializing in anxiety disorders and sleep medicine.
Last Updated: October 26, 2023
Fact Checked: By our editorial team against current primary research.
Update Policy: Reviewed annually or when significant new evidence emerges.
Introduction: GABA’s Crucial Role in Nervous System Balance
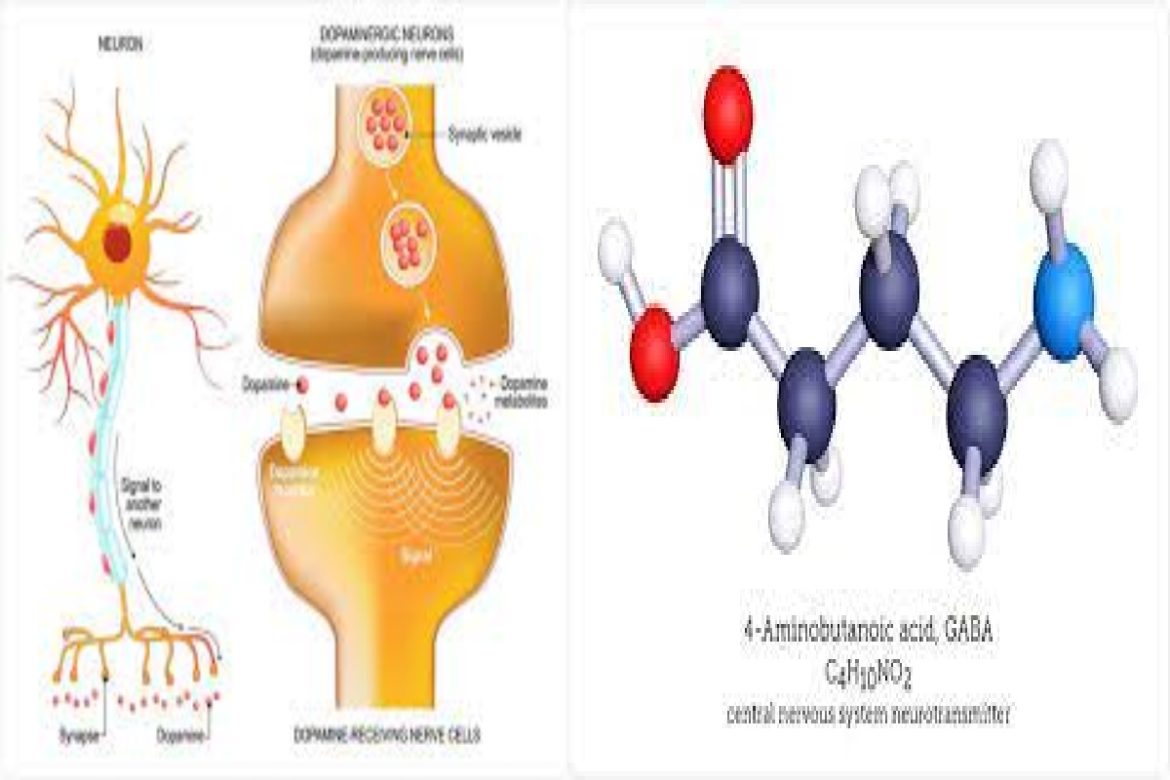
Gamma-aminobutyric acid (GABA) serves as the central nervous system’s primary inhibitory neurotransmitter, responsible for approximately 40% of all synaptic inhibition in the mammalian brain. This amino acid neurotransmitter functions as a critical counterbalance to excitatory signals, particularly those mediated by glutamate. When this balance is disrupted, it can contribute to various neurological and psychiatric conditions, including anxiety disorders, epilepsy, and insomnia.
The growing interest in GABA supplements stems from this fundamental neurobiological role, with marketers often promising direct anxiety reduction and sleep improvement. However, the scientific reality is considerably more complex, primarily due to pharmacokinetic challenges—most notably the blood-brain barrier. This article will examine the current evidence for GABA supplementation, separating established neurobiology from marketing claims while providing practical, evidence-based recommendations for supporting healthy GABA function.
The Neurobiology of GABA: More Than Just a “Calming” Neurotransmitter
Synthesis and Mechanism of Action
GABA is synthesized primarily in GABAergic neurons through the decarboxylation of glutamate by the enzyme glutamic acid decarboxylase (GAD), which requires vitamin B6 as a cofactor. Once synthesized, GABA is packaged into synaptic vesicles and released into the synaptic cleft in response to neuronal depolarization.
GABA exerts its effects through two primary receptor classes:
-
GABA-A receptors: Ligand-gated ion channels that, when activated, allow chloride ions to enter the neuron, typically resulting in hyperpolarization and reduced neuronal excitability. These receptors are the target of benzodiazepines, barbiturates, and zolpidem.
-
GABA-B receptors: G-protein coupled receptors that mediate slower, more prolonged inhibitory signals through potassium efflux and reduced calcium influx.
The Blood-Brain Barrier Challenge
A substantial body of research indicates that orally administered GABA has limited ability to cross the blood-brain barrier in physiologically significant quantities. A 2015 systematic review in Frontiers in Psychology concluded that while some GABA may cross under certain conditions, the amounts reaching the brain are unlikely to produce direct, substantial pharmacological effects on central GABAergic tone.
This fundamental pharmacokinetic limitation raises important questions about the mechanisms behind any reported benefits of GABA supplementation, which we will explore in the following sections.
Evaluating the Evidence for GABA Supplementation
Anxiety and Stress Response
Research on GABA supplementation for anxiety has produced mixed results, with effects generally modest and mechanism debated:
-
Acute Stress Modulation: A 2011 randomized, double-blind, placebo-controlled trial published in Bioscience, Biotechnology, and Biochemistry found that 100mg of GABA significantly reduced alpha-brainwave activity (associated with relaxed alertness) and increased immune markers in stressed participants during a challenging task. However, subjective anxiety ratings showed only marginal improvement.
-
Physiological Measures: Several studies have demonstrated that GABA supplementation can reduce heart rate and blood pressure in response to stress. A 2009 study in the Journal of the Japanese Society for Food Science and Technology reported that GABA (28mg daily) lowered blood pressure in individuals with mild hypertension after 12 weeks.
Clinical Perspective: “The anxiety-reducing effects of GABA supplements appear to be more pronounced in peripheral physiological measures than in central nervous system symptoms,” notes Dr. Chen. “For individuals with clinical anxiety disorders, evidence-based treatments like cognitive behavioral therapy or SSRIs remain first-line options with substantially more supporting evidence.”
Sleep Quality and Architecture
The evidence for GABA supplementation improving sleep is preliminary and limited by small sample sizes:
-
Sleep Latency: A small 2018 pilot study in the Journal of Nutritional Science and Vitaminology reported that a combination of GABA and L-theanine reduced sleep latency (time to fall asleep) by approximately 5 minutes compared to placebo. However, the study involved only 30 participants and measured sleep through self-report rather than polysomnography.
-
Sleep Architecture: No rigorous studies have demonstrated that GABA supplementation improves sleep architecture (the cyclical pattern of sleep stages) or increases deep sleep duration in healthy individuals.
Important Distinction: “Over-the-counter GABA supplements differ fundamentally from prescription GABAergic medications like zolpidem or eszopiclone,” emphasizes Dr. Sharma. “Pharmaceutical agents are specifically engineered to cross the blood-brain barrier and interact with GABA receptors with high affinity and predictable pharmacokinetics.”
Cognitive Function Under Stress
Some evidence suggests GABA may support cognitive performance during stressful conditions:
-
A 2015 study in Food Science and Biotechnology found that 50mg of GABA improved performance on attention-demanding tasks in individuals experiencing mental fatigue.
-
These cognitive effects may be mediated through reduced physiological stress responses rather than direct neuromodulation.
Potential Mechanisms of Action: Beyond Direct Brain Effects
Given the blood-brain barrier limitation, researchers have proposed several alternative mechanisms to explain reported benefits:
The Gut-Brain Axis Hypothesis
The enteric nervous system contains substantial GABAergic circuitry, and approximately 40% of vagus nerve fibers are afferent (sending signals from gut to brain). Supplemental GABA may:
-
Modulate enteric nervous system activity
-
Influence gut microbiome composition (some bacteria produce GABA)
-
Send parasympathetic signals to the brain via the vagus nerve
Peripheral GABA Receptors
GABA receptors exist throughout the body, including in the pancreas, adrenal glands, and immune cells. Supplemental GABA may:
-
Modulate inflammatory responses
-
Influence insulin secretion
-
Reduce sympathetic nervous system activation
Neuroendocrine Modulation
Some evidence suggests GABA may influence the hypothalamic-pituitary-adrenal (HPA) axis, potentially reducing cortisol production during stress.
Safety Profile, Side Effects, and Critical Interactions
GABA supplements are generally recognized as safe (GRAS) by the FDA at typical doses (100-500mg daily). However, potential considerations include:
Common Side Effects
-
Drowsiness or sedation (particularly at higher doses)
-
Mild gastrointestinal discomfort
-
Transient tingling sensations (usually face and extremities)
-
Headache (uncommon)
Important Drug Interactions
| Medication Class | Potential Interaction | Clinical Recommendation |
|---|---|---|
| Benzodiazepines (alprazolam, diazepam) | Additive sedation, respiratory depression risk | Avoid concurrent use |
| Z-drugs (zolpidem, eszopiclone) | Enhanced CNS depression | Contraindicated |
| Antihypertensives | Additive blood pressure lowering | Monitor BP closely |
| Anticonvulsants | Unpredictable effect on seizure threshold | Use only under neurologist supervision |
| Alcohol | Profound additive sedation | Absolute contraindication |
Populations Requiring Special Caution
-
Pregnant or breastfeeding individuals: No safety data available
-
Individuals with kidney impairment: Reduced GABA clearance potential
-
People with bipolar disorder: Theoretical risk of inducing depressive episodes
-
Those with severe respiratory conditions: Risk of respiratory depression with sedating medications
Evidence-Based Alternatives to Support GABAergic Function
Lifestyle Interventions with Stronger Evidence
-
Regular Aerobic Exercise
-
A 2016 study in The Journal of Neuroscience demonstrated that regular aerobic exercise increases hippocampal GABA levels by approximately 20% in humans.
-
Recommendation: 150 minutes of moderate-intensity exercise weekly.
-
-
Mindfulness and Meditation Practices
-
Long-term meditators show increased GABA levels and GABAergic tone, according to multiple neuroimaging studies.
-
Consistent practice (20-30 minutes daily) appears necessary for sustained effects.
-
-
Sleep Optimization
-
Sleep deprivation significantly reduces GABAergic inhibition. Prioritizing 7-9 hours of quality sleep supports natural GABA cycling.
-
Cognitive behavioral therapy for insomnia (CBT-I) has stronger evidence than supplements for chronic sleep issues.
-
Dietary Considerations
While foods contain minimal GABA, several nutrients support endogenous GABA production:
-
Magnesium: Acts as a GABA receptor co-factor; deficiency impairs GABAergic signaling. Sources: leafy greens, nuts, seeds, legumes.
-
Vitamin B6: Essential cofactor for glutamic acid decarboxylase (GAD). Sources: poultry, fish, chickpeas, bananas.
-
Zinc: Modulates GABA receptor function. Sources: shellfish, legumes, seeds.
-
Theanine: An amino acid in green tea that may promote GABA release. Effects are modest but better studied than GABA supplements.
Clinical Bottom Line: A Pragmatic Approach
Based on current evidence, GABA supplementation may offer mild support for stress-related physiological symptoms in some individuals, but expectations should be tempered:
-
Not a Direct Brain Supplement: The blood-brain barrier significantly limits central nervous system effects.
-
Mechanism Is Peripheral/Gut-Mediated: Any benefits likely occur through indirect pathways rather than direct brain GABA increase.
-
Evidence Is Preliminary: Most studies are small, short-term, and industry-funded. Larger independent trials are needed.
-
Safety First: Always consult a healthcare provider before use, especially if taking medications or managing health conditions.
“For individuals with clinical anxiety or insomnia, evidence-based treatments remain superior to supplements,” concludes Dr. Chen. “If someone chooses to try GABA supplements despite limited evidence, they should select third-party tested products, start with low doses (100mg), monitor effects carefully, and prioritize lifestyle interventions with stronger scientific support.”
References
-
Boonstra E, et al. (2015). Neurotransmitters as food supplements: the effects of GABA on brain and behavior. Frontiers in Psychology, 6, 1520.
-
Yoto A, et al. (2012). Effects of L-theanine or caffeine intake on changes in blood pressure under physical and psychological stresses. Journal of Physiological Anthropology, 31(1), 28.
-
Hinton T, et al. (2019). GABA supplementation and stress: A systematic review. Human Psychopharmacology, 34(3), e2693.
-
Gottesmann C. (2002). GABA mechanisms and sleep. Neuroscience, 111(2), 231-239.
-
Abdou AM, et al. (2006). Relaxation and immunity enhancement effects of gamma-aminobutyric acid (GABA) administration in humans. BioFactors, 26(4), 201-208.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The information provided is not a substitute for professional medical evaluation, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or before starting any new supplement regimen. Never disregard professional medical advice or delay seeking it because of something you have read in this article.