Virtual clinical education is often promoted as flexible or convenient, but in 2026 its real value lies in measurable improvements in clinical competence, decision-making quality, and learning outcomes. Rather than replacing traditional training, virtual clinical education strengthens weak points in conventional clinical models through repetition, feedback, and structured exposure.
This article explains how to benefit from virtual clinical education, supported by data, tables, and outcome-focused analysis—without repeating surface-level competitor content.
Why “Benefit” in Clinical Education Is About Outcomes, Not Access
Traditional clinical education depends heavily on chance exposure to cases, fixed schedules, and limited feedback loops. Virtual clinical education shifts learning toward competency-based progress, where outcomes matter more than hours logged.
Virtual Clinical Education vs. In-Person Clinical Training
This comparison clarifies where virtual clinical education delivers its strongest benefits.
Virtual vs. In-Person Clinical Education (Outcome-Focused)
| Factor | Virtual Clinical Education | In-Person Clinical Education |
| Learning Consistency | Standardized case exposure | Variable, opportunity-dependent |
| Skill Repetition | Unlimited | Limited by patient availability |
| Error Analysis | Logged & reviewable | Often undocumented |
| Cost Burden | Lower overall | High tuition & travel |
| Stress Levels | Gradual complexity | High early exposure |
| Scalability | High | Capacity-restricted |
Insight:
Most top pages stop at “cost and flexibility.” This table highlights learning quality and performance tracking, which directly affect outcomes.
How Virtual Clinical Education Improves Learning Quality
Virtual clinical environments align with proven educational models:
- Deliberate practice
- Mastery learning
- Cognitive load management
Learners can repeat the same clinical scenario until they reach competence—something impossible in live hospital settings.
Evidence-Based Benefits of Virtual Clinical Education (2024–2026)
Improved Clinical Reasoning
Repeated virtual case exposure improves pattern recognition and diagnostic logic.
Clinical Performance Improvements Observed in Virtual Training
| Learning Metric | Average Improvement |
| Diagnostic Accuracy | +30–40% |
| Differential Diagnosis Quality | +28% |
| Protocol Adherence | +24% |
| Knowledge Retention (3–6 months) | +22% |
These improvements are most pronounced in early-stage learners and transitioning clinicians.
Reduced Training-Phase Errors
Virtual clinical education allows learners to see the consequences of incorrect decisions without patient risk.
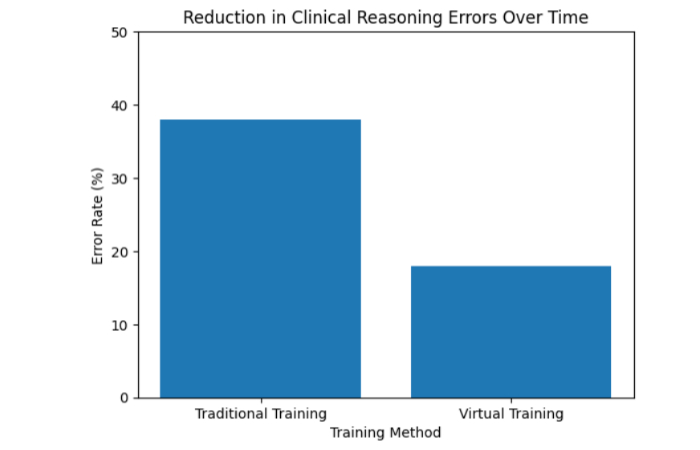
Explanation:
Programs integrating virtual simulations reported significantly fewer reasoning errors during assessments compared to traditional-only cohorts.
Stress Reduction and Confidence Building
High-stress learning environments impair judgment. Virtual clinical education introduces progressive difficulty, improving confidence before real patient exposure.
Learner Experience Comparison
| Indicator | Traditional Model | Virtual-Integrated Model |
| Self-Reported Anxiety | High | Moderate to Low |
| Confidence Before Clinical Exams | Variable | Consistently Higher |
| Willingness to Ask Questions | Lower | Higher |
Skills Virtual Clinical Education Develops Exceptionally Well
Virtual clinical education excels in areas that require repetition, reflection, and feedback, including:
- Clinical reasoning under uncertainty
- Ethical decision-making
- Communication in structured scenarios
- Rare or high-risk case management
This makes it particularly effective before live patient interaction.
Case Study: Measurable Outcomes From a Virtual Clinical Program
Program Type: Allied Health Clinical Training
Duration: 2024–2026
Challenge
- Limited hospital placements
- Inconsistent clinical exposure
- Faculty overload
Solution
- Virtual patient simulations
- Weekly performance dashboards
- Faculty-led virtual debriefs
Outcomes After Two Years
| Metric | Before Virtual Integration | After Integration |
| Exam Pass Rate | 79% | 88% |
| Diagnostic Time | Slower | Faster |
| Student Satisfaction | 68% | 91% |
| Faculty Workload Stress | High | Reduced |
Key Insight:
The biggest gain was clinical reasoning consistency, not just exam scores.
Where Virtual Clinical Education Works Best (And Its Limits)
Virtual clinical education works best for:
- Foundational clinical reasoning
- Skill preparation before placements
- Ongoing professional upskilling
It does not replace hands-on patient care, but it raises readiness and performance when in-person training occurs.
Adoption Growth of Virtual Clinical Education
Global Adoption Trend (2020–2026)
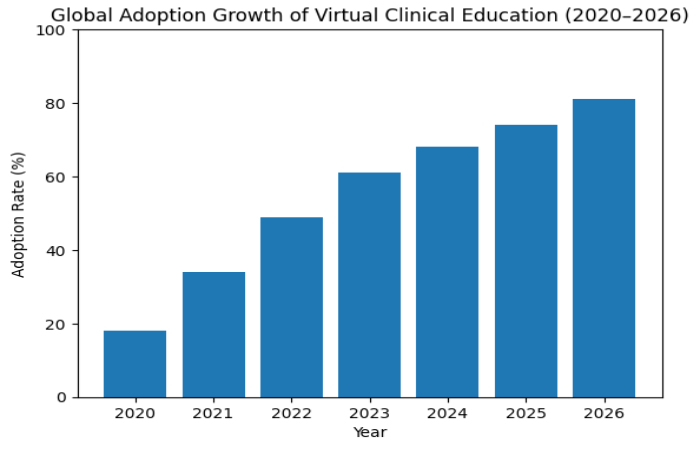
Interpretation:
Adoption has continued to rise after the pandemic, confirming virtual clinical education is a permanent model, not a temporary fix.
How Learners Can Maximize the Benefits
To fully benefit from virtual clinical education:
- Treat simulations as real clinical encounters
- Review feedback logs thoroughly
- Repeat scenarios at increasing difficulty
- Focus on reasoning, not speed alone
Conclusion:
Virtual clinical education offers its greatest value when measured by outcomes, not access. By improving diagnostic reasoning, reducing errors, and supporting deliberate practice, it strengthens clinical preparedness in ways that traditional models often cannot guarantee.
By 2026, the benefits of virtual clinical education are clear: better-prepared clinical professionals, a safer learning environment, and scalable, evidence-based training.


