Many people explore new tools to help with weight and metabolic health. Zepbound is one option some clinicians may discuss alongside nutrition, activity, and behavior changes. Understanding how it fits within a broader plan can support safer, more informed choices.
Before making decisions, you can learn more about Zepbound usage and safety and discuss whether it aligns with your health goals. Consider how it may interact with existing conditions, daily routines, and long-term strategies for weight and blood sugar management.
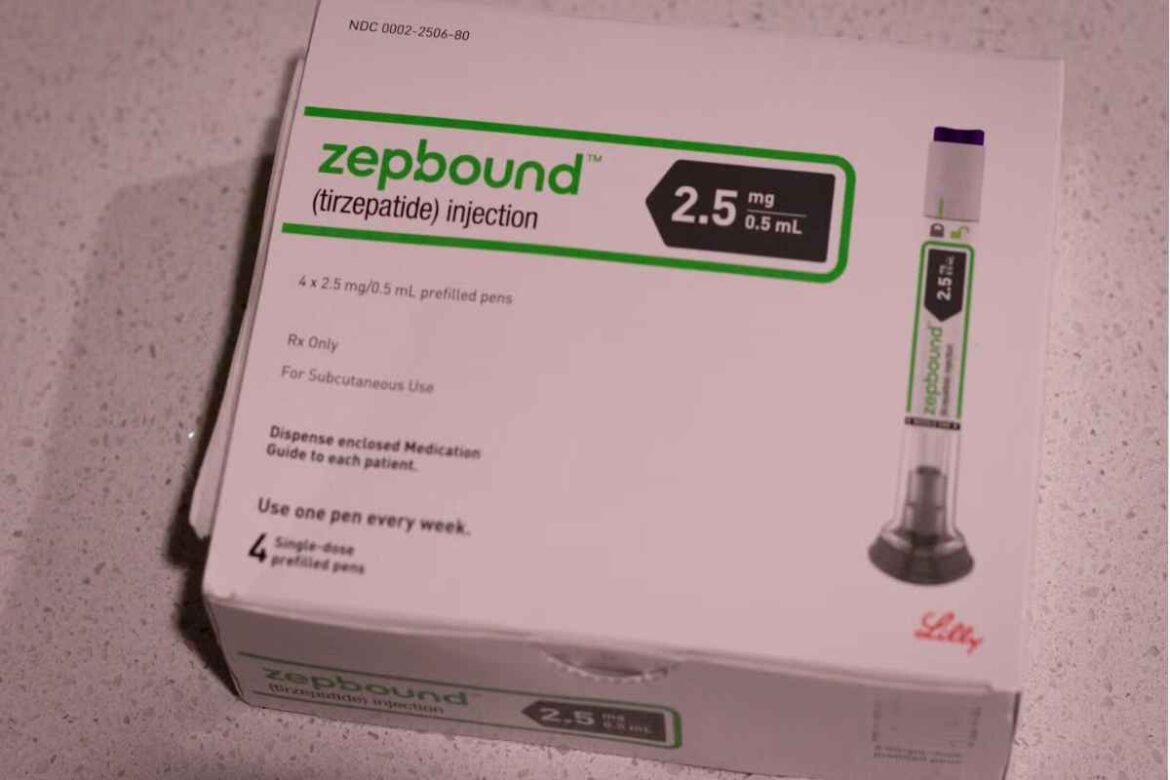
What Zepbound Is and How It Fits In
Zepbound is a prescription therapy that targets pathways involved in appetite, fullness, and glucose control. It is generally considered within comprehensive programs that include nutrition, physical activity, sleep, and stress management. For many, it is a support tool rather than a standalone solution.
People living with overweight or obesity often face complex, overlapping challenges. These include hunger signals, environmental triggers, and medical conditions like type 2 diabetes. Zepbound may help some individuals reduce calorie intake and improve metabolic markers when used with lifestyle changes.
Who Might Consider Zepbound
Clinicians may discuss Zepbound with adults who have obesity, or those with overweight and weight-related complications. These complications can include high blood pressure, abnormal cholesterol, sleep apnea, fatty liver disease, or joint strain. Some individuals with prediabetes or type 2 diabetes might also be considered, depending on overall risk.
Eligibility depends on personal health history, medications, and readiness for sustained lifestyle changes. A shared decision-making approach helps set realistic goals and timelines. Regular follow-up allows dose adjustments, monitoring, and support for behavior changes.
Potential Benefits and Realistic Expectations
Potential benefits may include reduced hunger, earlier fullness, and gradual weight loss. Some people also see improvements in waist circumference, blood pressure, and blood sugar levels. Results vary, and plateaus are common even with good adherence.
Setting expectations helps maintain motivation. Track progress beyond the scale, including energy, sleep quality, mobility, and lab values. Zepbound works best when paired with consistent routines and problem-solving when life gets busy.
How Zepbound May Work
Many newer weight therapies act on gut–brain signaling. They can influence hormones involved in appetite and post-meal glucose control. By lowering hunger and slowing digestion, they may support a calorie deficit with fewer cravings.
This mechanism intersects with diabetes pathways where insulin resistance and elevated glucose are common. When paired with nutrition strategies, the combined effect can support metabolic health. Your clinician can explain how this fits with any diabetes or prediabetes plan.
Safety, Side Effects, and Cautions
Common side effects include nausea, vomiting, diarrhea, constipation, and abdominal discomfort. These often improve as the body adapts, especially with careful dose escalation. Eating smaller, slower meals and limiting heavy, high-fat foods may help.
Less common risks may include gallbladder issues, pancreatitis, or allergic reactions. People with certain endocrine tumors or a family history of related cancers may be advised against use. Always share your full medical history and all medicines, including supplements.
If you experience severe abdominal pain, persistent vomiting, signs of dehydration, or allergic symptoms, seek urgent care. Discuss pregnancy plans, fertility, or breastfeeding with your clinician before starting. Safe disposal and storage of injectable devices are also important.
Nutrition Strategies That Complement Therapy
Aim for balanced, satisfying meals with protein, fiber, and healthy fats. This combination helps manage hunger and stabilizes energy between meals. Hydration supports digestion and may reduce nausea.
Example patterns include vegetables, beans or lentils, lean proteins, whole grains, nuts, and seeds. Practical steps: plan two to three core breakfasts, rotate simple lunches, and batch-cook proteins and vegetables. Gentle portion awareness and mindful eating can further support fullness cues.
Physical Activity and Daily Routines
Regular movement supports weight maintenance, mood, and blood sugar control. Start with low-impact activities such as brisk walking, cycling, or swimming. Add resistance training 2–3 times weekly to preserve muscle mass.
Track steps or minutes, and set incremental goals. Short activity breaks during long sitting periods can improve glucose levels. Consistent sleep and stress reduction also help regulate appetite signals.
Monitoring Progress and Adjusting the Plan
Plan periodic check-ins to review weight trends, side effects, and adherence. Labs may include A1C, fasting glucose, lipids, and liver enzymes depending on your profile. Communicate changes in appetite, mood, or gastrointestinal symptoms.
Expect adjustments. Doses may change, or schedules may be modified to improve tolerance. If progress stalls, revisit nutrition patterns, activity, and sleep before assuming the therapy no longer helps.
Special Considerations for Diabetes and Prediabetes
For people with type 2 diabetes, weight reduction can improve insulin sensitivity. This may allow changes in other diabetes medications over time. Monitor for low blood sugar if you take insulin or insulin-stimulating drugs.
Coordinate closely with your diabetes care team. A structured plan supports safe adjustments and consistent targets. Education around hypoglycemia signs and sick-day rules remains essential.
When Zepbound May Not Be Appropriate
Certain medical histories or current conditions may limit suitability. These include some gastrointestinal diseases, pancreatitis history, or specific endocrine disorders. Individuals with severe kidney or liver disease require careful evaluation.
Personal preference also matters. Not everyone wants injections, medical monitoring, or potential side effects. Explore alternatives and choose the approach you can sustain.
Everyday Tips for Side-Effect Management
- Eat small, slow meals; pause between bites.
- Favor lean protein, cooked vegetables, and lower-fat options.
- Limit alcohol and very rich, fried, or spicy foods early on.
- Sip fluids through the day; consider ginger or peppermint tea.
- Schedule doses at consistent times; track symptoms in a log.
Building a Supportive Environment
Prepare your kitchen with nutrient-dense staples and ready-to-eat produce. Plan ahead for travel, social events, and holidays. Identify non-food rewards for milestones.
Consider peer support, coaching, or counseling to manage stress and triggers. Small, steady habits typically beat short-term intensity. Over time, routines become automatic and less effortful.
Exploring Broader Weight Management Resources
Weight changes are easier to maintain with a comprehensive approach. Nutrition, activity, sleep, behavior tools, and clinical care all play a role. Learn about structured programs and tools in Weight Management resources to see what fits your needs.
Key Questions to Ask Your Clinician
- Based on my history, am I a good candidate for Zepbound?
- How will we measure progress beyond the scale?
- What side effects should prompt a call or visit?
- How could Zepbound interact with my current medications?
- What is our plan if I plateau or want to stop?
Bottom Line
Zepbound can be a helpful tool for some people when paired with consistent lifestyle habits. It is not a quick fix, and careful monitoring matters. An individualized, sustainable plan is the best foundation for long-term health.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
For broader health topics, resources, and clinical insights, visit CanadianInsulin.